It was an emotional roller coaster getting insurance to approve my DBS surgery, since it was for dystonia. DBS is an effective treatment for Parkinson’s, which is approved by insurance on a regular. The success for dystonia isn’t cut and dry. It tends to be more effective for people with DYT1 genetic mutations but it’s not a cure all. I understood it could help me along with my current treatment of medication and injections.
The date finally came, October 1, 2018! I was super excited!
Then came the denial letter. I had a serious, ugly meltdown. I knew that meant long term disability. Uh, hello, I was too young. This was impossible. The dystonia was getting worse by the day. I couldn’t afford my treatments and medication without insurance, let alone only 60% of my salary. For the first, I lost hope. I didn’t have much of a future ahead of me.
My doctors and their staff fought the denial and surgery was back on. I’m ever so grateful for all of them. I held my breathe until the actual day. I was worried insurance would pull the rug out from under me again.
The hardware consists of a neurotransmitter placed below the collarbone. It’s the battery-powered pacemaker portion of everything. The lead is the wire with electrodes on the end. The extension connects the neurotransmitter to the leads.
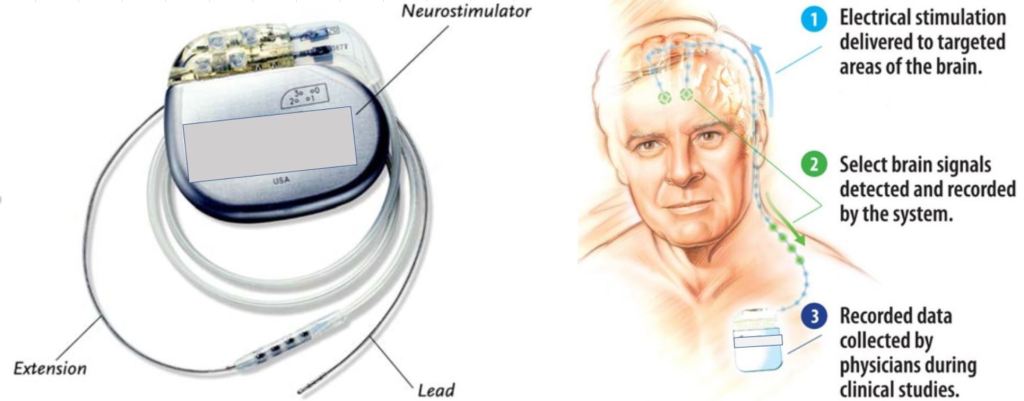
There was a new hardware system from St Jude, marketed by Abbot. It has four electrodes and the middle two electrodes have segments that can send a more precise pulse for better programming of the brain. It was so new that there was no sample available for my surgery consultation.
My consultation was with a Medtronic, which is the most widely used at the time. It has the same four electrodes without segmental control. They do have a lot of neurotransmitter options like a rechargeable battery model. They were fairly compact like the size of a zippo lighter.
I met with the neurosurgeon and found out the St Jude model wasn’t approved for use of surgery in the MRI machine. This was a big deal because the game plan was to implant the wires both sides in one surgery while asleep. The alternative is an awake surgery and they would only do one side at a time. I would have to be awake to complete tasks when the wire is a critical point which could affect motor functions. The asleep method newer and is more accurate.
I met with the neurosurgeon and found out the St Jude model wasn’t approved for use of surgery in the MRI machine. This was a big deal because the game plan was to implant the wires both sides in one surgery while asleep. The alternative is an awake surgery and they would only do one side at a time. I would have to be awake to complete tasks when the wire is at a critical point which could affect motor functions. The asleep method is newer and is more accurate.
Because of my occipital neuralgia, the neurosurgeon really wanted me asleep since the halo bolted to my head during surgery sits almost on top of the occipital nerve. If the St Jude device wasn’t approved by the time of surgery, we would use the Medtronic device. Yay, one way or another, I would be asleep!
